Anterior ischemic optic neuropathy (AION) is a disease of
micro-circulation of the optic nerve head. Although arteritic AION is related
with Giant cell arteritis, non-arteritic AION (NAION) is associated with small
crowded discs, optic disc drusen, hypertension, diabetes, hyperlipidemia and
smoking. NAION with optic disc drusen occurs at an earlier age. Vascular supply
is compromised due to drusen in already small discs. Presence of optic disc
drusen is an incidental finding but there is evidence that patients report
transient visual obscurations as a result of increased pressure in the optic
nerve head. We present a case of bilateral optic disc drusen with unilateral NAION.
The effect of a single injection of intravitreal Bevacizumab is discussed in
this case report.
CASE REPORT
A fifty years old Asian male presented
with sudden onset of decreased vision in left eye. He also complained of
transient obscuration of vision in the last few months. He was known
hypertensive and non-diabetic. There was history of familial hyperlipidemia and
transient ischemic attacks. The patient suffered left hemiparesis in 2005 and
he had undergone left cholesteotoma surgery three times in the past (latest in
year 2000).
The patient was an average stature, average built male and
general physical examination showed no systemic abnormality. He was orthotropic
with best-corrected visual acuity of 6/9 in right eye and 6/60 in left eye. Color
vision was disturbed in left eye. Extra ocular movements were normal with no
pain on eye movements. There was left RAPD and slit lamp examination for
anterior segment showed +1 nuclear sclerosis in each eye. Intra ocular
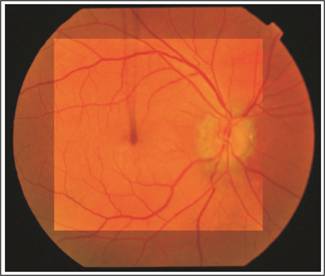
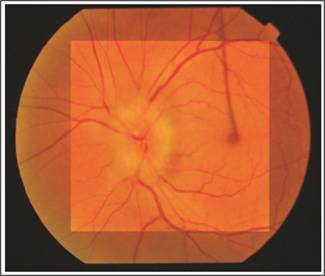
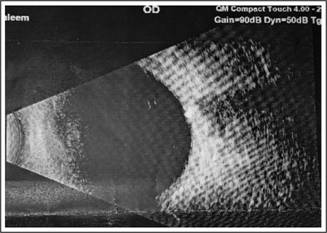
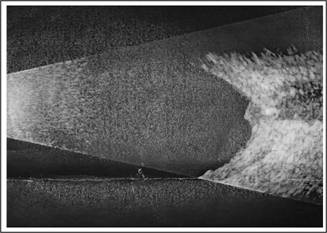
pressures were 13 mm Hg in each eye. Fundus examination revealed bilateral macular
drusen. Optic disc drusen were also seen in both eyes and optic disc edema in
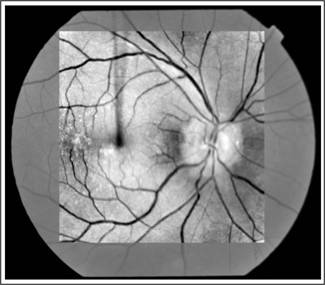
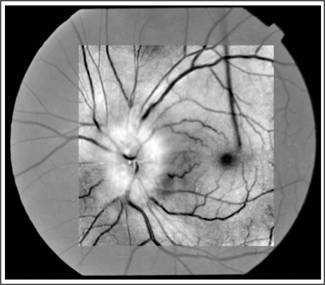
left eye. Optic disc drusen were confirmed on B-scan and red free fundus
photographs. OCT showed inferior RNFL defect in right eye while in left eye
there was thickening of RNFL indicating disc edema. Blood work up was
unremarkable (CBC, ESR, LFTs, RFTs). Serum cholesterol was normal but triglycerides
were high (524.2 mg/dl). ECG and Echocardiography were normal. Carotid Doppler was
normal. CT angio showed tiny calcific atheromatous plaques in distal portion of
left common carotid artery and proximal left internal carotid artery with
normal lumen. The patient was given an intravitreal injection of Bevacizumab
1.25 mg in 0.05 ml. There was no improvement in visual status after three months
of follow up.
DISCUSSION
NAAION is associated with hypertension, diabetes and
hyperlipidemia. Other associations include, migraine, use of oral
contraceptives, anemia and use of antihypertensive medicines at bed time. This particular
patient had systemic as well as ocular risk factors for NAION; hyperlipidemia,
hypertension, small crowded discs and optic disc drusen. Optic disc drusen with
co-existing vascular risk factors in a patient of NAAION was also reported by
Deborah and Sharon1. Although optic disc drusen are asymptomatic but
they can lead to complications including NAION. Optic disc drusen can also
cause
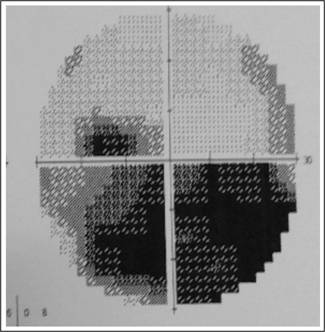
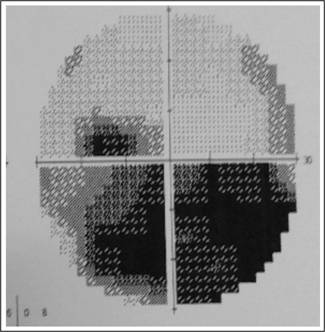
Fig. 4: Inferior Altitudnal visual field defect in NAAION
and optic disc drusen.
CRAO and CRVO due to small scleral
canal and crowding of retinal nerve fibers in the optic disc.
NAAION with optic disc drusen occurs at
a younger age as was seen in our patient whose age was 50 years. Ayhan Z has
reported NAION with bilateral optic disc drusen in a 46 years old patient2.
The youngest patient reported to have NAION with optic disc drusen was of 12
years3. Other authors have also reported optic disc drusen with
NAION.4 Purvin et al in a case series showed that patients with
NAION with optic disc drusen have transient visual obscurations5. This
finding was consistent with our patient who had transient obscuration of vision
and transient ischemic attacks before he developed optic neuropathy. Although
Purvin reported better visual prognosis in such patients, our patient had poor
visual outcome after three months of follow up. This particular patient had inferior altitudinal visual field loss
which is seen in 55 to 80% cases of NAION6.
Hypertension can have a direct effect
on optic disc blood supply as well as indirect effect, caused by nocturnal
hypotension due to antihypertensive drugs taken at bed time.
Use of anti VEGF agents in retinal
diseases has become wide spread all over the world. Its use in the treatment of
NAION is also reported in literature but with variable results. It is
hypothesized that anti-VEGFs decrease disc edema thus resulting in decrease
pressure on optic nerve fibers and better visual outcome. But the results are
inconsistent. Some authors showed visual
improvement after injecting intravitreal anti-VEGF for NAION7. Others showed no visual improvement in vision after intravitreal
anti-VEGF injection8. This was similar to our result. Still there
are other reports which found no difference between bevacizumab and natural
history for change in visual field, visual acuity, or optic nerve OCT thickness9.
One case report showed definitive promising results where NAION was related
with macular edema10. This can be explained by the fact that the
visual loss caused by macular edema was corrected with anti-VEGF which has
shown promising results in macular edema cases.
Few case reports are not enough evidence
for use of anti-VEGF in NAION. Further clinical trials are needed to see the
role of these agents in optic nerve diseases.
CONCLUSION
Optic disc drusen are important risk factor for development
of NAION in younger patients, even in the absence of vascular risk factors.
However, these patients should be kept at close watch for earlier and timely management
of vascular factors like hypertension, diabetes, migraine, hyperlipidemia and
anaemia etc. Role of anti-VEGF in this condition is still a question mark.
Authors Affiliation
Dr. Muhammad Khalil
FCPS, Professor of ophthalmology Lahore medical and dental
college
Dr. Tayyaba Gul Malik
FCPS, Professor of ophthalmology, Rashid Latif Medical
college
Role of Authors
Dr. Muhammad Khalil
Data
acquisition, analysis, Data compiling and manuscript drafting.
Dr. Tayyaba Gul Malik
Data
acquisition, analysis, Data compiling and manuscript drafting.
REFERENCES
1.
Deborah KL, Sharon LC. Acute visual loss in a patient with
optic disc drusen. Clin Ophthalmol. 2013; 7: 795–799.
2.
Ayhan Z, Yaman A, Bajin MS, Saatci AO. Unilateral Acute Anterior Ischemic Optic Neuropathy in a Patient with an
Already Established Diagnosis of Bilateral Optic Disc Drusen. Case Rep Ophthalmol
Med. 2015; 4.
3.
Nanji AA, Klein KS, Pelak VS, Repka MX. Nonarteritic anterior ischemic optic
neuropathy in a child with optic disk drusen. J AAPOS. 2012; 16: 207–9.
4.
Megur, D. Megur, U. Megur, and S.
Reddy. Anterior ischemic optic neuropathy in association with optic
nerve head drusen. Indian J Ophthalmol. 2014; 62 (7): 829–31.
5.
Purvin V, King R, Kawasaki A, Yee R. Anterior ischemic optic neuropathy in
eyes with optic disc drusen. Arch
Ophthalmol. 2004; 122: 48–53.
6.
Traustason OI, Feldon
SE, Leemaster JE, Weiner JM. Anterior ischemic optic neuropathy:
classification of field defects by Octopus automated static perimetry. Graefes Arch Clin Exp
Ophthalmol. 1988; 226: 206–12.
7.
Saatci AO, Taskin O,
Selver OB, Yaman A, Bajin MS. Efficacy of intravitreal ranibizumab
injection in acute nonarteritic ischemic optic neuropathy: A long-term follow
up. Open Ophthalmol J. 2013; 7: 58-62.
8.
Pece A, Querques G,
Quinto A, Isola V. Intravitreal ranibizumab injection for
nonarteritic ischemic optic neuropathy. J Ocul Pharmacol Ther. 2010; 26: 523-7.
9.
Rootman DB, Gill HS,
Margolin EA. Intravitreal bevacizumab for the treatment of
nonarteritic anterior ischemic optic neuropathy: A prospective trial. Eye,
2013; 27: 538-44.
10.
Dave VP, Pappuru RR. An unusual presentation of nonarteritic
ischemic optic neuropathy with subretinal fluid treated with intravitreal
bevacizumab. Indian J Ophthalmol. 2016; 64 (1): 87-8.